Are you concerned about long recovery times and visible scars from gynecological surgery? Maybe you’re trying to plan around work, kids, or caring for family, and the idea of being “out of action” for weeks feels impossible. It’s also normal to worry about safety, pain, and cost, especially when you’ve never had surgery before.
If you’ve been asking yourself, “Why choose laparoscopic surgery for gynecology?” you’re not alone. This minimally invasive, keyhole surgery approach often helps you heal faster and feel more comfortable, with smaller cuts and a shorter hospital stay for many patients.
What Is Laparoscopic Gynecological Surgery ?
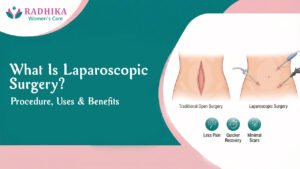
Laparoscopic surgery uses a few small cuts (often around 0.5 to 1 cm) instead of one larger incision. Your surgeon places a thin camera (a laparoscope) through one small opening and uses tiny instruments through the others, all while you’re under anesthesia. The camera shows a magnified view on a screen, which can help the surgeon work with care.
In Laparoscopic vs open gynecological surgery, the biggest difference is incision size. Smaller incisions usually mean less tissue disruption, which often translates to less pain and a quicker return to routine.
Benefits of Laparoscopic Surgery for Women’s Health
When you’re in pain or dealing with heavy bleeding, you don’t just want “a procedure.” You want your life back, with the least disruption possible. The benefits of laparoscopic surgery often line up with what you care about most: comfort, recovery, and getting back to your normal rhythm.
A real-world trend supports that shift. In recent years, outpatient hysterectomy has become more common, with reports showing outpatient rates rising from about 17% to 44% as minimally invasive techniques expanded. That doesn’t mean every case is outpatient, but it shows how strongly practice has moved toward shorter stays when appropriate.
Here’s how Laparoscopic surgery for women’s health can help:
- Smaller incisions, less “pull” on your body: Many patients feel they can move more comfortably sooner because there’s less disruption to the abdominal wall.
- Less post-op discomfort for many patients: Pain control still matters, but smaller cuts often mean fewer days of strong pain medicine.
- Lower chance of some wound-related issues: A smaller surface wound may reduce the risk of certain problems like wound infection for some patients.
- Shorter hospital stay in many cases: Depending on the procedure and your health, you may go home the same day or within 1 to 2 days.
- Back to routine sooner: Recovery time after gynecological laparoscopy is often shorter than with open surgery, though it varies by procedure, fitness, and your job demands.
- Clearer view for careful work: The camera’s magnified image can support precision surgery, especially in delicate pelvic areas.
One simple comparison to keep in mind: open surgery can be the right choice in some situations, but it typically involves a larger incision, which often means a longer recovery and more soreness at the incision site.
The Advantages of laparoscopic gynecological surgery are strongest for many patients when the procedure is planned well and performed by an experienced surgeon. It’s not “risk-free,” but it’s widely viewed as safe for the right patient and the right condition.
Minimal Scarring and Better Cosmetic Results
Small cuts usually heal into smaller marks. For you, that can mean less worry when you dress, exercise, or look in the mirror. It can also mean less tenderness around the incision once healing is underway.
Think of it like fixing something through a small access panel instead of removing an entire wall. The goal is still a strong repair, with less visible impact on the outside.
Less Pain and Faster Healing
Because the cuts are smaller, your muscles and skin are often less disturbed. Many people notice they can stand upright, walk around, and do light tasks sooner than they expected.
Typical recovery is often quicker than open surgery, but it still depends on what you have done (for example, cyst removal versus hysterectomy) and your body’s healing pace.
Lower Risk of Some Complications
For some patients, laparoscopy is linked with a lower risk of certain issues such as wound infection, heavy bleeding, or slower wound healing. At the same time, every surgery has risks, including anesthesia-related risks, and your surgeon should explain what applies to your case.
A helpful safety fact: for hysterectomy, reports suggest about 6% of laparoscopic cases may need conversion to open surgery if safety requires it. That possibility is part of good planning, not a failure.
Shorter Hospital Stay and Quicker Return to Daily Life
A shorter stay matters when you’re juggling a job, a household, and people who rely on you. Many patients can return to gentle daily activity sooner, and some can resume desk work earlier than after an open procedure.
You still need rest. But for many women, laparoscopy makes recovery feel more like a steady walk back to normal, not a long pause in life.
Precision Surgery With Advanced Technology
The camera view can magnify small structures, which helps surgeons see tissue planes more clearly. That matters in the pelvis, where nerves, blood vessels, the bowel, bladder, ovaries, and uterus sit close together.
This is where “advanced” doesn’t have to sound scary. It simply means the surgeon can work with a clearer view and fine tools, supporting careful steps and controlled movements during precision surgery.
Read also : What Is Laparoscopic Surgery? Procedure, Uses & Benefits
Common Gynecological Problems Treated With Laparoscopy
Laparoscopy for gynecology can be used to diagnose a problem, treat it, or both. In some cases, it helps confirm a diagnosis when scans don’t give the full picture. In other cases, it allows treatment during the same procedure.
Common reasons your doctor may discuss Gynecological laparoscopic surgery include:
- Ovarian cysts: Cyst removal (cystectomy) may be possible while preserving healthy ovarian tissue.
- Fibroids: Myomectomy (fibroid removal) can be considered for symptom relief and fertility goals in selected cases.
- Endometriosis: Laparoscopy may help find and treat endometriosis lesions that drive pain.
- Ectopic pregnancy: In some situations, laparoscopy may be used when urgent surgical care is needed.
- Pelvic adhesions (scar tissue): Adhesiolysis may reduce pulling pain in carefully chosen patients.
- Hysterectomy options: Some hysterectomies can be done with a laparoscopic approach, depending on anatomy and medical needs.
Fibroids, Endometriosis, and Ovarian Cysts
Fibroids are non-cancerous growths in the uterus, endometriosis is tissue similar to the uterine lining growing outside the uterus, and ovarian cysts are fluid-filled sacs on the ovary. You may hear procedures like myomectomy for fibroids and cystectomy for cysts. Laparoscopic gynecological surgery can sometimes treat these with smaller incisions, depending on size, location, and your health.
Pelvic Pain, Abnormal Bleeding, and Hysterectomy Options
Pelvic pain can be confusing because it can come from several causes, sometimes at the same time. Laparoscopy may help identify causes that don’t show clearly on imaging. If hysterectomy is on the table, the approach is personal and guided by your doctor, your symptoms, and your long-term plans.
Why Choose Radhika Women’s Care for Laparoscopic Surgery?
When you’re choosing surgery, you’re also choosing a team and a process. At Radhika Women’s Care, you can expect an experienced, expert approach with clear communication, so you understand what’s happening and why. You also get careful planning, including a pre-op evaluation, a step-by-step explanation of your procedure, and structured follow-up.
If you’re comparing options online, you might see searches like “best laparoscopic surgeon” or. Those searches make sense, but the best choice is the surgeon and center that fit your condition, explain options clearly, and make you feel safe and heard.
Radhika Women’s Care is located in Adajan surat. If you’re researching from Surat or elsewhere, ask about practical planning for visits and follow-ups.
Conclusion
If you’re weighing surgery for a gynecological problem, it helps to focus on what recovery will really look like. Many women choose Laparoscopic Surgery because it often means small cuts, less pain for many patients, faster healing, a shorter stay, and a quicker return to daily life, with the added benefit of a clear camera view for careful work.